What is IBS?
Irritable bowel syndrome (IBS) is a functional disorder (so there are no specific structural problems) of the gut-brain axis that affects the large colon or bowel, and it is characterised by abdominal pain, discomfort, and changes in bowel habits (constipation, diarrhoea or both). IBS affects 3.5% Australians and 5-10% of people worldwide and there are three main subtypes:
- IBS-C (constipation) shows up as abdominal cramping, pain and bloating, particularly after eating. Bowel habits can often alternate between being constipated to having normal bowel motions.
- IBS-D (diarrhoea) – can present as the urgent and uncontrollable need to have a bowel motion, and possible incontinence. There can be pain and discomfort and there can be significant disruption to quality of life from this.
- IBS-M (mixed, alternating constipation and diarrhoea)
What are other common IBS symptoms?
- Distension (enlargement of the stomach area)
- Bloating (like an inflated balloon or pregnant belly look)
- Gas (wind, farts, pops, flatulence or whatever you call it!)
- Urgency to defecate- urgency of poo’s
- Pencil poo’s (thin poo’s, this can be a sign of other conditions too though)
- Fatigue (because of other symptoms)
Diagnosis- Could it be something else?
Getting a diagnosis is important to rule out other health problems such as endometriosis, coeliac disease, inflammatory bowel disease (IBD), gut allergies or intolerances, and infections. Speaking to your health professional they can often make a diagnosis asking some questions from a set of criteria called Rome IV.
Also, small intestinal bacterial overgrowth or (SIBO) also has similar symptoms to IBS, and it is possible to have both. If you have an overlap of symptoms your health practitioner may order a breath test first to rule out SIBO.
Red flags that might need investigation
- Being over 40 and a family history of bowel cancer or inflammatory bowel disease
- Unintentional weight loss
- Blood in stools
- Recent change in bowel habits when over 50 years
- Iron deficiency anaemia on blood test
- Faecal occult blood test result is positive
- Bowel motions at night
What causes IBS?
It is not exactly known what causes IBS, but triggers can include stress, medication, infections and diet. Research shows other causes could be hypersensitivity in the lining of the gut, changes in the gut microbiome, altered gut motility (how fast or slow the gut is) and low grade intestinal inflammation. Often though you might notice it starts after a bout of ‘gastro’ (gastroenteritis) or a stressful event or even a bout of antibiotics or other medication.
Common food triggers
Certain foods and drinks can trigger IBS, so avoiding or reducing these foods can be helpful:
- Lactose (milk sugar) containing foods (milk, some yoghurts, ice-cream)
- Alcohol
- Gas forming foods such as onion, garlic, brussel sprouts, cabbage, cauliflower, dried beans and lentils
- Artificial sweeteners (sorbitol, mannitol, aspartame)
- Caffeine
- Gluten- hypersensitivity can mimic IBS
What are the common treatments?
There are a range of treatment options for IBS, although not all of them are specific to treating IBS and may be more targeted at managing the symptoms. However, dietary changes such as low FODMAPS and reducing trigger foods have been shown to improve symptoms significantly.
- Medications – drugs such as antispasmodics have been used for decades as it was thought spasms caused IBS. Anti-depressants have been used and can relieve some symptoms but have side effects. Also, antibiotics, laxatives and anti-diarrhoeal medications can help with symptoms but do not treat or heal the condition.
- Dietary changes- research has shown eliminating foods that exacerbate IBS can reduce symptoms. There are now many studies that support low FODMAP diets for IBS symptoms (more on that later!)
- Fibre insoluble fibre is more likely to aggravate IBS especially pain and bloating. However, psyllium husks which are a soluble fibre can improve symptoms especially in IBS-C. Fibres that produce less gas such as psyllium, oats, linseeds, sterculia and methylcellulose are better tolerated in IBS. Whereas, wheat bran and inulin may worsen IBS symptoms.
- Probiotics- Lactobacillus plantarum 299va strain of lactic acid bacteria has been shown in a number of studies to reduce abdominal pain, flatulence, bloating and normalise stool frequency in IBS patients.
- General tips the UK’s National Institute of Health Care and Excellence (NICE) has guidelines that also produce significant improvements in IBS-D. They recommend having smaller frequent meals. Plus avoiding excess alcohol, caffeine, and trigger foods.
- Exercise and yoga- inactive people with IBS more prone to constipation may benefit from regular gentle exercise although excessive strenuous exercise may aggravate symptoms in some people. Yoga has shown benefits for IBS symptoms as it is thought the poses, breathing techniques and meditation help.
- Gut directed hypnotherapy a recent study compared the effect of gut directed hypnotherapy to the low FODMAP diet and found it gave similar relief to IBS symptoms. The therapist should specialise in the gut and IBS.
So, what is low FODMAPS?
FODMAPs stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. Essentially, they are types of sugars or short-chained carbohydrates that are fermentable and poorly absorbed in the gut. When FODMAPS pass through the small intestine they attract water and as they move into the large intestine they start to ferment, which produces gas. So, then the extra gas and water leads to bloating and stretching of the gut wall. People with IBS are hypersensitive to this, and it causes a lot of pain and discomfort.
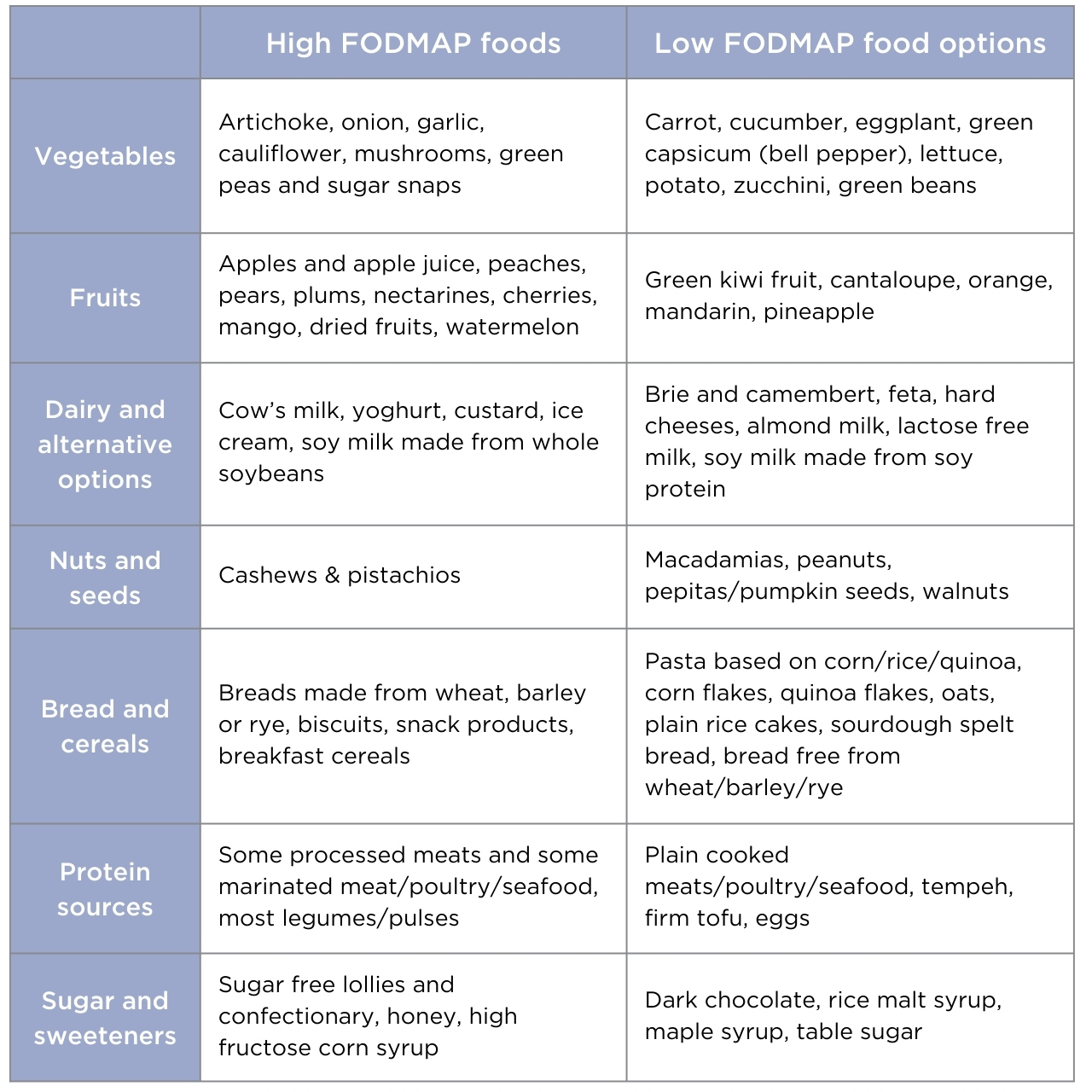
Researchers at Monash University in Victoria, Australia were the first to discover the low FODMAPS diet and to research which foods are high in FODMAPS and low in FODMAPS (See Table 1).
Table 1. High and low FODMAP FOODS adapted from Monash University.
Who should do a low FODMAPS diet?
Only people who are medically diagnosed with IBS should do a low FODMAP diet, as the diet isn’t a diet for life and has been designed to do for 2-6 weeks to challenge certain foods to see if they are triggers for IBS and exclude them with the guidance of a health practitioner. The low FODMAP diet is low in certain nutrients and is designed more to figure out trigger foods.
Key take home points
IBS should be diagnosed to rule out other conditions and can be managed by a range of treatments, some of which will work for some and not for others. So, it is important to get the guidance of a health practitioner. Some tips for managing IBS include having smaller frequent meals, avoiding trigger foods (which may involve a low FODMAPS diet). Avoiding excess alcohol, caffeine and artificial sweeteners. Keeping foods that cause gas to a minimum, such as onion, garlic, brussel sprouts, cabbage, cauliflower, dried beans and lentils.
Other options are to include some daily fibre (especially for IBS-C) and probiotics (containing Lactobacillus plantarum 299v), and think about exercise, yoga or gut directed hypnotherapy for stress management.





